Published: 25/05/23 12:00 Categories: Microbiology
What do we know about Campylobacter?
The genus Campylobacter comprises small, curved or spiral-shaped, gram-negative bacilli and most species exhibit corkscrew-like movement by means of a flagellum polar at one or both ends of the bacterium. Importantly, they have oxidase activity, do not form spores and are microaerophilic (grow best with low oxygen concentration).
Thermophilic species of the genus Campylobacter can grow between 37-42ºC, which is why they are commonly found in animals, especially birds, which have a higher body temperature than mammals.

Discovering pathogenic Campylobacter species
Currently, the Campylobacter genus comprises 17 species and six subspecies. Of these, the following are pathogenic in humans Campylobacter jejuni and Campylobacter coli, and less frequently C. lari, C. upsaliensis and C. fetus.
Among the virulence factors that allow the bacteria to cause damage to host cells are flagella-mediated motility, adherence to the intestinal mucosa, invasive and inflammatory capacity and, finally, the ability to produce toxins, such as CDT toxin (cytolethal distension toxin), which is frequently produced by gram-negative bacteria gram-negative bacteria. This toxin, through its DNase activity, prevents cell mitosis and, as a consequence, leads to cell death.
How does Campylobacter come to infect humans?
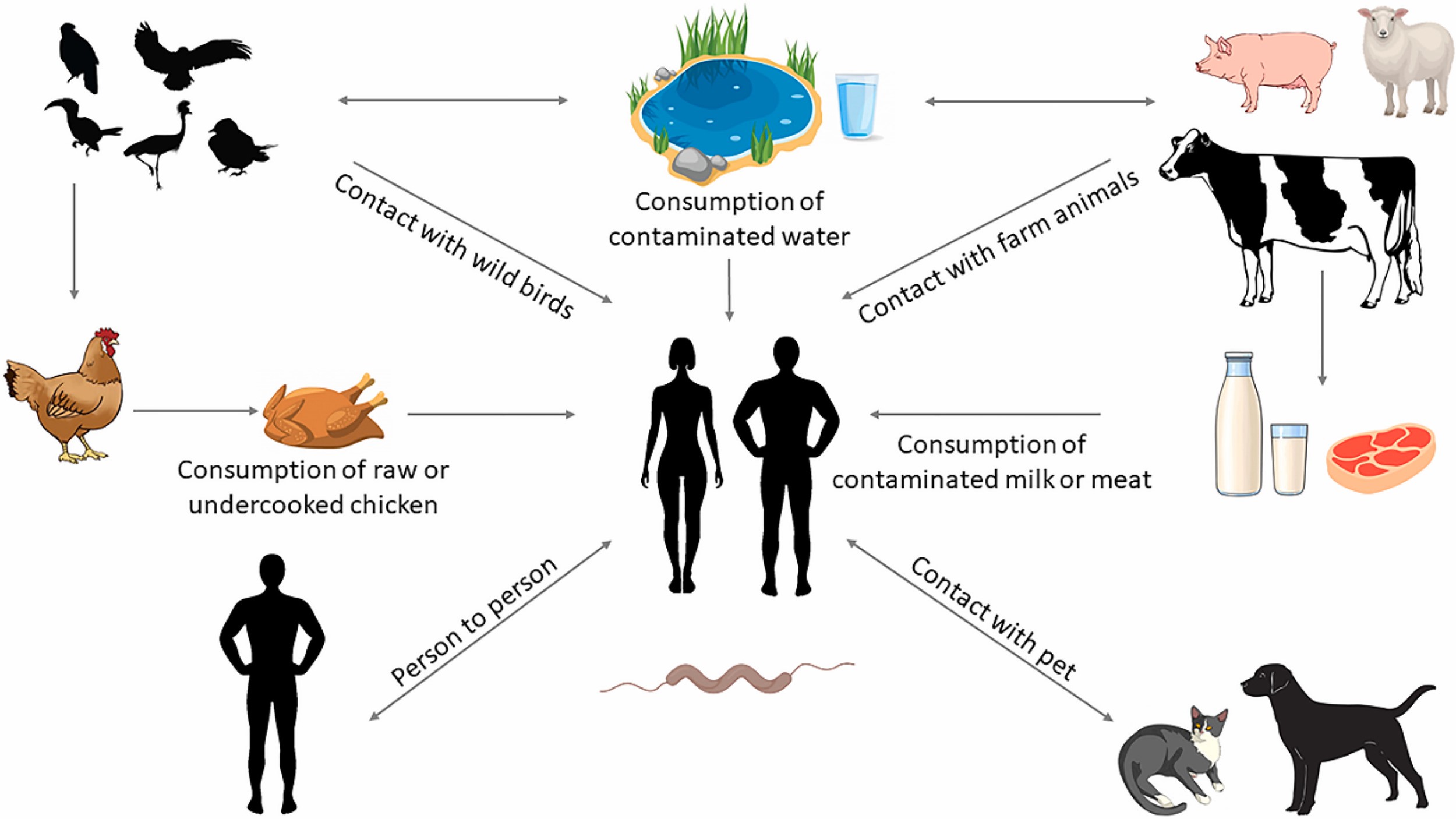
Campylobacter species are commonly found in the intestine of healthy wild and domestic animals, such as poultry, cattle, pigs, sheep, and in companion animals, such as dogs and cats. Therefore, campylobacteriosis is considered to be a zoonosis, i.e. a disease transmitted to humans by animals or animal products that may be contaminated by feces. Contaminated water, usually from feces, can also be a source of infection.
Disease and treatment
Campylobacteriosis presents with symptoms such as diarrhea (often bloody), fever and abdominal pain. In rare cases, the infection can lead to serious complications such as sepsis, reactive arthritis or neurological disorders such as Guillain-Barré syndrome.
Treatment is generally not necessary, except for fluid and electrolyte replacement. Antimicrobial treatment is recommended in invasive cases (when bacteria invade intestinal mucosal cells and damage tissues) or to suppress the carrier state.
Antimicrobial resistance
The antibiotic resistance in Campylobacter is an emerging global problem and has been recognized by the WHO as a serious public health serious public health problem. Although there are variations among different strains and different geographic regions, most are resistant to antibiotics such as fluoroquinolones, tetracycline and erythromycin. The cause of this resistance lies in the indiscriminate use of antibiotics in animal production for decades to control, prevent and treat infections, and enhance animal growth.
Actions by regulatory agencies regarding the incidence of Campylobacter
Campylobacteriosis is the most reported zoonotic disease in the EU, followed by salmonellosis, with more than 246,000 human cases per year according to the latest report of the European Food Safety Agency (EFSA), fortunately with a mortality rate of 0.03%. The highest incidence was detected in chicken meat (37.5%) and turkey meat (28.2%).
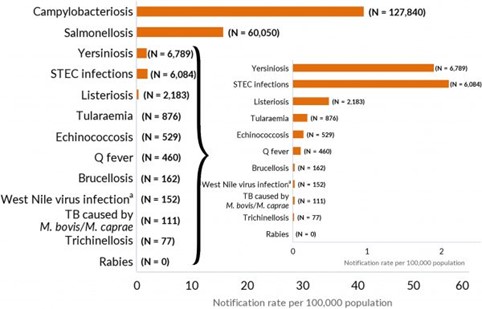 Number of reported cases (N) and notification rates of confirmed human zoonoses in the EU, 2021 (per 100,000 population -x-axis). Source: The European Union One Health 2021 Zoonoses Report. EFSA Journal, 20(12), e07666.
Number of reported cases (N) and notification rates of confirmed human zoonoses in the EU, 2021 (per 100,000 population -x-axis). Source: The European Union One Health 2021 Zoonoses Report. EFSA Journal, 20(12), e07666.
In recent years, there has been an increase in the number of Campylobacter monitoring and control plans on poultry farms, especially in fattening chickens, including the implementation of biosecurity measures, regular testing of poultry for Campylobacter and the adoption of proper handling practices to reduce meat contamination during production and processing.

In addition, importance is given to consumer awareness campaigns, including information on safe handling of raw food, thorough cooking and good kitchen hygiene to prevent or reduce the risk posed by these contaminated foods.
The reference method for the detection and detection and enumeration of Campylobacter spp. in food samples is ISO 10272. You can find all Condalab solutions for your analysis on our website, and we invite you to watch our CondalabTalk Campylobacter and its impact on human health.

 Condalab Says YES to the World’s Leading Lab Trade Fair: Analytica 2026
Condalab Says YES to the World’s Leading Lab Trade Fair: Analytica 2026
 CONDALAB to Exhibit at WHX Labs Dubai 2026
CONDALAB to Exhibit at WHX Labs Dubai 2026
 Food fraud: How do we detect it?
Food fraud: How do we detect it?
 Visit Us at MEDICA 2025 – Discover Our Precise Detection Solutions
Visit Us at MEDICA 2025 – Discover Our Precise Detection Solutions
 PCR: The Technique Revolutionizing Rapid Detection in the Food Industry
PCR: The Technique Revolutionizing Rapid Detection in the Food Industry